MiR-122-5p inhibits the epithelial mesenchymal transition of liver cancer cells by inducing hiPSCs to differentiate into hepatocyte-like cells
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
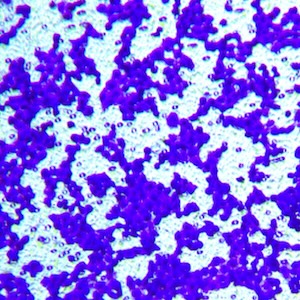
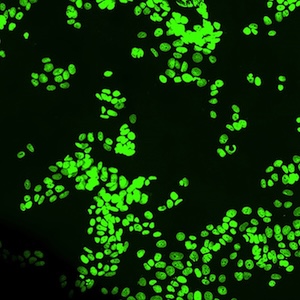
Epithelial-mesenchymal transition (EMT) is closely linked to liver cancer prognosis, invasiveness, and aggressiveness. One promising treatment for liver cancer is cell therapy, where stem cells are stimulated to develop into functional liver cells. This study aimed to investigate the effect of miR-122-5p on the differentiation of human induced pluripotent stem cells (hiPSCs) into hepatocyte-like cells and its impact on the EMT process in liver cancer cells. MiR-122-5p was overexpressed or silenced in hiPSCs to analyze the expression of liver-specific markers, including AFP, ALB and ASGPR, to confirm hepatocyte-like differentiation. A co-culture system with HepG2 liver cancer cells was also used to evaluate the effect of miR-122-5p-overexpressing hiPSCs or miR-122-5p-silencing hiPSCs on the expression of EMT markers. Results revealed that overexpression of miR-122-5p in hiPSCs induced hepatocyte-like characteristics, as evidenced by increased levels of AFP, ALB, and ASGPR. However, knockdown of miR-122-5p had the opposite effect. In the co-culture system, hiPSCs overexpressing miR-122-5p inhibited the EMT process of HepG2 cells, resulting in increased levels of mesenchymal markers and decreased levels of epithelial markers. Taken together, miR-122-5p promotes the differentiation of hiPSCs into hepatocyte-like cells and inhibits EMT process of liver cancer cells. Targeting miR-122-5p may be a novel approach to prevent liver cancer progression through cell therapy.
Supporting Agencies
this study was supported by the Tianjin Health Bureau Funded ProjectHow to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.